M
Mayenne Perpetua
Guest
Visit [CCO] Certification Coaching Organization LLC for more articles about [CCO] Certification Coaching Organization LLC - Medical Certifications - Learn It - Get Certified - Stay Certified.
Q: Are Emergency Department visits diagnoses which state “suspected,” “presumed,” etc., to be coded following the inpatient or outpatient guidelines? That is, are coders to follow inpatient guidelines of “confirmed” if the patient is admitted through the ED to Observation/Inpatient status and use the outpatient guidelines of “not confirmed” if the patient is discharged from ED to home? Can you please give me directions on this?
A: That is a great question. When we take a look at this, a couple of things to remember, the question confused a few things: you got to remember what areas of the hospital are considered outpatient hospital departments. Both the Emergency room and Observation status, even if the patient is “admitted” to observation, that is still considered an outpatient part of the hospital. Those outpatient departments are required to follow the Section IV guidelines in the ICD-10 manual. Those are the guidelines for Diagnostic Coding and Report Guidelines for Outpatient Service.
According to that, most facilities – just to give you an idea of what happens in most facilities – if a patient presents to the emergency room, those emergency room charges are entered into the system. And guess what, they actually get put into the same system, if you will, as the charges that are used to generate your inpatient claim. If we have a patient come into the ER whether they’re discharged and sent home or admitted to the inpatient facility, they get put in to the hospital billing system, and so do the inpatient charges that the patient is admitted.
VIDEO: Emergency Department Visits Diagnoses Medical Coding Guidelines
When the claim is generated, they then look to see what place of service did that patient wind up in to determine which rules do we need to follow. If they wind up in the inpatient environment, they were admitted for a full hospitalization, the claim that’s generated is going to utilize the inpatient diagnosis, quite frankly. It is going to code for all of the different pieces that it needs to.
As an ER coder or an ED coder, what you need to do is remember that regardless of where the patient winds up, your services is part of the hospital outpatient department and you have to code those accordingly, so you’re going to follow those Section IV guidelines.
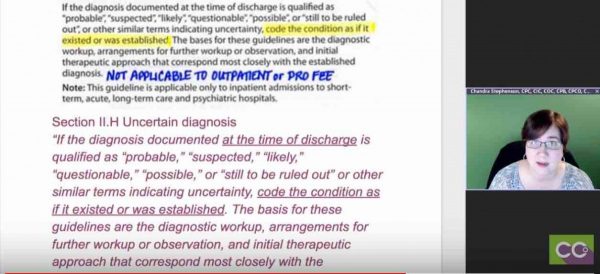
When it comes to uncertain diagnoses, which is what this question started with: What do I do with those probable, suspected, likely, rule out, all of those? The guidelines are specific. What I did was I pasted in a picture of the guidelines directly from my coding manual, that’s why they’re all marked up and then I typed up the same thing. In case it came out blurry or you had trouble reading it, you can actually see it typed as well.
 What those guidelines say is if you’re coding for the hospital outpatient department, you do not code for any diagnoses that is documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis” or anything else that indicate uncertainty; so no “probable,” “likely,” “suspected,” anything like that.
What those guidelines say is if you’re coding for the hospital outpatient department, you do not code for any diagnoses that is documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis” or anything else that indicate uncertainty; so no “probable,” “likely,” “suspected,” anything like that.
Instead, what you do is you code what the highest degree of certainty was that the provider knew during that ER visit, what did they know? Maybe they only knew the patient had abdominal pain, that’s all you could code. They haven’t figured out yet what else was going on with the patient, so you’re going to code whatever it is you know. That can be signs and symptoms, that can be abnormal test results, it could be any other reason for the visit if you don’t have a definitive diagnosis. That’s if you’re coding for the hospital outpatient department like the emergency room.
What do you do if you’re the inpatient coder? We ask this question from an ER perspective, but what happens if I’m an inpatient coder and I’m coding for the facility charges inside the hospital? Quick designation I want to make, a lot of people confused inpatient and outpatient and they think, “Oh, outpatient is the doctor, inpatient is the hospital.” No. We’re talking about different places of service.
The physician services, those are what we call our professional services, our pro fees, and that doctor can provide services on either place. They can work in their office or they can work in the hospital. Either way, they are considered an outpatient entity, they have to follow the outpatient rules because we’re not billing, they’re not billing for the hospital.
The hospital has two different sets of rules, either we have the outpatient departments like we just talked about with the ER, or we’re billing for the inpatient services, the full admission where we’re billing for room and board and lights and all of the equipment that we use and everything else. Well, if you’re an inpatient coder billing for the facility, your roles are different. Instead of Section IV, which is what the outpatient and the physician’s follow, in the inpatient hospital environment you follow the Section II guidelines, and those tell you what to do.
They say specifically under Section II.H, it says Uncertain Diagnosis. If you’re coding for the inpatient hospital facility, you are going to take what the diagnosis says at the time of discharge. Not at the time they’re admitted, but right when we send them home, that discharge summary.
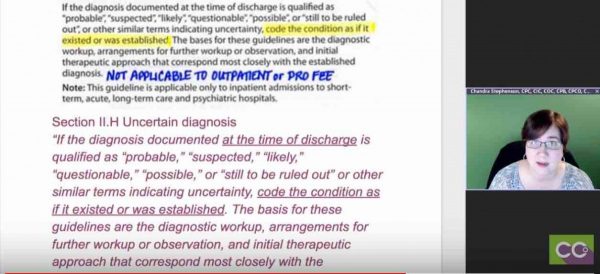 What did we know? If it was “probable,” “suspected,” “likely,” “questionable,” “possible,” any uncertain term, you get to code it as though it existed. You code it just like it was an established condition. If it says “possible appendicitis” you code it as appendicitis.
What did we know? If it was “probable,” “suspected,” “likely,” “questionable,” “possible,” any uncertain term, you get to code it as though it existed. You code it just like it was an established condition. If it says “possible appendicitis” you code it as appendicitis.
The reason for this is, when we’re billing in the inpatient facility environment, we are billing for the services that it took to rule in or rule out that diagnosis. It doesn’t matter whether the patient has appendicitis or not. If we’re trying to figure out whether they have it, we’re going to use the same amount of resources to rule it in as we would to rule it out. That’s the only reason this differ.
The other reason that they differ, if I’m billing for the facility, I can assign a diagnosis that says “rule out appendicitis,” I can call it appendicitis and it never attaches to my patient. It simply says we used all of the services that we needed to rule out appendicitis. If I attach it from an outpatient or a physician perspective, that diagnosis attaches to the patient because we’ve said it’s a confirmed diagnosis, that’s what the guideline says. If I were to assign something that the patient did not actually have, I was still trying to figure out, rule it out, I could wind up putting something they never had on their record and it’s very, very difficult to then get that removed and that creates all sorts of problems for the patient down the road. Worst case scenario, we accidentally assign a cancer diagnosis or heart attack diagnosis to a patient who never had either. That could prevent them from getting life insurance, all sorts of issues.
That’s why you need to remember when you’re coding for these, if I’m coding for the inpatient facility, I follow the Section II rule that says: “Hey! I can code those ‘probable,’ ‘suspected,’ ‘likely,’ ‘rule out.’” If I’m coding for the outpatient hospital or I’m coding for the physician, oh no those attached to the patient and I follow the Section IV guidelines that say I cannot use those. If you’re an ED coder or an ER coder, your hospital outpatient facility and you got to remember when you got a probable, a suspected, a likely or any kind of uncertain diagnosis, we cannot code for those. I think that wraps that one up.
Laureen: I just wanted to say, too, for people that are seeing Chandra’s notes, many people are familiar with CCO’s bubbling and highlighting technique, this is Chandra’s version of annotation; and so, the same way that we make available my entire CPT manual, to see all of the notes, we’re doing the same with Chandra’s ICD-10 manual. That’s very valuable, so if you’re a full student of ours, you get access to that. I just wanted to throw that in there and her handwriting is a lot neater than mine.
Related Emergency Department Visits Diagnoses Posts:
The post Emergency Department Visits Diagnoses Medical Coding Guidelines appeared first on [CCO] Certification Coaching Organization LLC.
Continue reading...
Q: Are Emergency Department visits diagnoses which state “suspected,” “presumed,” etc., to be coded following the inpatient or outpatient guidelines? That is, are coders to follow inpatient guidelines of “confirmed” if the patient is admitted through the ED to Observation/Inpatient status and use the outpatient guidelines of “not confirmed” if the patient is discharged from ED to home? Can you please give me directions on this?
A: That is a great question. When we take a look at this, a couple of things to remember, the question confused a few things: you got to remember what areas of the hospital are considered outpatient hospital departments. Both the Emergency room and Observation status, even if the patient is “admitted” to observation, that is still considered an outpatient part of the hospital. Those outpatient departments are required to follow the Section IV guidelines in the ICD-10 manual. Those are the guidelines for Diagnostic Coding and Report Guidelines for Outpatient Service.
According to that, most facilities – just to give you an idea of what happens in most facilities – if a patient presents to the emergency room, those emergency room charges are entered into the system. And guess what, they actually get put into the same system, if you will, as the charges that are used to generate your inpatient claim. If we have a patient come into the ER whether they’re discharged and sent home or admitted to the inpatient facility, they get put in to the hospital billing system, and so do the inpatient charges that the patient is admitted.
VIDEO: Emergency Department Visits Diagnoses Medical Coding Guidelines
When the claim is generated, they then look to see what place of service did that patient wind up in to determine which rules do we need to follow. If they wind up in the inpatient environment, they were admitted for a full hospitalization, the claim that’s generated is going to utilize the inpatient diagnosis, quite frankly. It is going to code for all of the different pieces that it needs to.
As an ER coder or an ED coder, what you need to do is remember that regardless of where the patient winds up, your services is part of the hospital outpatient department and you have to code those accordingly, so you’re going to follow those Section IV guidelines.
When it comes to uncertain diagnoses, which is what this question started with: What do I do with those probable, suspected, likely, rule out, all of those? The guidelines are specific. What I did was I pasted in a picture of the guidelines directly from my coding manual, that’s why they’re all marked up and then I typed up the same thing. In case it came out blurry or you had trouble reading it, you can actually see it typed as well.

Instead, what you do is you code what the highest degree of certainty was that the provider knew during that ER visit, what did they know? Maybe they only knew the patient had abdominal pain, that’s all you could code. They haven’t figured out yet what else was going on with the patient, so you’re going to code whatever it is you know. That can be signs and symptoms, that can be abnormal test results, it could be any other reason for the visit if you don’t have a definitive diagnosis. That’s if you’re coding for the hospital outpatient department like the emergency room.
What do you do if you’re the inpatient coder? We ask this question from an ER perspective, but what happens if I’m an inpatient coder and I’m coding for the facility charges inside the hospital? Quick designation I want to make, a lot of people confused inpatient and outpatient and they think, “Oh, outpatient is the doctor, inpatient is the hospital.” No. We’re talking about different places of service.
The physician services, those are what we call our professional services, our pro fees, and that doctor can provide services on either place. They can work in their office or they can work in the hospital. Either way, they are considered an outpatient entity, they have to follow the outpatient rules because we’re not billing, they’re not billing for the hospital.
The hospital has two different sets of rules, either we have the outpatient departments like we just talked about with the ER, or we’re billing for the inpatient services, the full admission where we’re billing for room and board and lights and all of the equipment that we use and everything else. Well, if you’re an inpatient coder billing for the facility, your roles are different. Instead of Section IV, which is what the outpatient and the physician’s follow, in the inpatient hospital environment you follow the Section II guidelines, and those tell you what to do.
They say specifically under Section II.H, it says Uncertain Diagnosis. If you’re coding for the inpatient hospital facility, you are going to take what the diagnosis says at the time of discharge. Not at the time they’re admitted, but right when we send them home, that discharge summary.
The reason for this is, when we’re billing in the inpatient facility environment, we are billing for the services that it took to rule in or rule out that diagnosis. It doesn’t matter whether the patient has appendicitis or not. If we’re trying to figure out whether they have it, we’re going to use the same amount of resources to rule it in as we would to rule it out. That’s the only reason this differ.
The other reason that they differ, if I’m billing for the facility, I can assign a diagnosis that says “rule out appendicitis,” I can call it appendicitis and it never attaches to my patient. It simply says we used all of the services that we needed to rule out appendicitis. If I attach it from an outpatient or a physician perspective, that diagnosis attaches to the patient because we’ve said it’s a confirmed diagnosis, that’s what the guideline says. If I were to assign something that the patient did not actually have, I was still trying to figure out, rule it out, I could wind up putting something they never had on their record and it’s very, very difficult to then get that removed and that creates all sorts of problems for the patient down the road. Worst case scenario, we accidentally assign a cancer diagnosis or heart attack diagnosis to a patient who never had either. That could prevent them from getting life insurance, all sorts of issues.
That’s why you need to remember when you’re coding for these, if I’m coding for the inpatient facility, I follow the Section II rule that says: “Hey! I can code those ‘probable,’ ‘suspected,’ ‘likely,’ ‘rule out.’” If I’m coding for the outpatient hospital or I’m coding for the physician, oh no those attached to the patient and I follow the Section IV guidelines that say I cannot use those. If you’re an ED coder or an ER coder, your hospital outpatient facility and you got to remember when you got a probable, a suspected, a likely or any kind of uncertain diagnosis, we cannot code for those. I think that wraps that one up.
Laureen: I just wanted to say, too, for people that are seeing Chandra’s notes, many people are familiar with CCO’s bubbling and highlighting technique, this is Chandra’s version of annotation; and so, the same way that we make available my entire CPT manual, to see all of the notes, we’re doing the same with Chandra’s ICD-10 manual. That’s very valuable, so if you’re a full student of ours, you get access to that. I just wanted to throw that in there and her handwriting is a lot neater than mine.
Related Emergency Department Visits Diagnoses Posts:
- Correct Coding Sequence of Vaccine Administration Codes
- Which Credential is the Best After CPC? | Medical Coding Advice
- ICD 10 Impact on Risk Adjustment | Risk Adjustment Training
The post Emergency Department Visits Diagnoses Medical Coding Guidelines appeared first on [CCO] Certification Coaching Organization LLC.
Continue reading...
